Iowa woman, 27, has 99% chance of developing dementia: ‘I needed to know’
Alyssa Nash inherited the gene mutation for FTD, a rare form of early-onset dementia — but here's why she has hope for her future
Alyssa Nash, 27, of Northern Iowa, is a healthy, energetic young woman with a bright smile and a deep love for her family. She enjoys ceramics, painting and working as a receptionist at a local hospital.
But underneath her happy exterior, Nash carries a quiet fear of turning into someone she no longer recognizes.
Seven years ago, when she was just 20, Nash learned she's a carrier for a gene mutation that can cause FTD (frontotemporal dementia), an early-onset neurodegenerative disease that most commonly impacts people as early as their 30s, 40s and 50s.
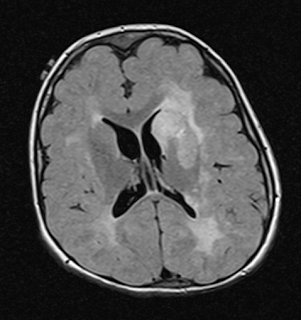
FTD is marked by the degeneration of the frontal and/or temporal lobes of the brain, according to the Association for Frontotemporal Degeneration (AFTD).
Much less common than Alzheimer’s disease, FTD currently affects some 60,000 people in the U.S.
Symptoms can start as early as 21 years old, but most cases occur between the ages of 45 and 64, per the AFTD.
Common signals of the disease include personality changes, difficulty speaking and understanding language, trouble with decision-making and a lack of empathy.
Dr. Tiffany Chow, neurologist and vice president of clinical development at the biotechnology company Alector in South San Francisco, California, is an expert in this type of dementia.
"Unlike Alzheimer's disease, FTD causes a drastic turnaround."
"FTD is one of the most fascinating neurodegenerative diseases because it actually affects your personality," she told Fox News Digital in an interview.
"Unlike Alzheimer's disease, FTD causes a drastic turnaround," Chow said. "So the nicest people become the most obnoxious people. It's a marked difference that affects everything in terms of how the world perceives you and how you perceive the world."
From a clinical standpoint, FTD is devastating to families, the doctor said.
"These are people who are mainly in their late 40s or 50s," she said. "They're still working and may be very active in their community. They're still raising children. And so in some ways, the impact is much greater economically and in terms of the ripple effects on the people around them."
It’s a challenge that Nash knows all too well. Her father began to display signs of FTD when he was only 38 years old, just as Nash was entering high school.
A long road to diagnosis
"The biggest challenge was seeing him change completely into someone else and become someone I never thought he could be," Nash told Fox News Digital in an interview. "And having to grow up in that atmosphere — it was tough."
It was seven years before Nash’s father was officially diagnosed.
"We went through years of unknowns and questions," Nash said.
Along with her mother and brother, Nash helped care for her dad as his dementia progressed, even as she struggled to hide his condition from everyone at her high school.
"It was this big secret I was keeping," she said. "I basically had two lives. I didn’t tell anyone at school because I didn't want to be different — I wanted to feel normal, in a sense."
She added, "But then I'd have to go home right away to help take care of my dad and make sure he was OK."
Delayed diagnoses are common
The majority of dementia cases — more than 60%, studies show — are not diagnosed for a host of reasons, according to Diane Ty, senior director of the Milken Institute Center for the Future of Aging in Washington, D.C.
And by the time they are identified, the condition has usually progressed to the later stages, she said.
Ty had a similar experience when her own father began exhibiting symptoms of dementia.
"We should be doing cognitive testing as part of primary care."
"We confused some of the behavioral challenges that we were seeing as the effects of him taking early retirement and being depressed, but in retrospect, it was the early stages of dementia," she said during a discussion with Fox News Digital.
In most cases, Ty said, it’s not until there is some sort of accident or incident that the affected person is brought in for testing.
"That’s just not acceptable," she said. "We should be doing cognitive testing as part of primary care, not unlike getting a mammogram or a colonoscopy. It should be part of the annual wellness visit."
Ty added, "We are not regularly looking at our brain health. I think that's one of the biggest barriers to timely detection and diagnosis."
Genetic screening: ‘I needed to know’
In some cases, FTD can be passed down from a parent to a child.
"We have made a lot of progress in determining the genetic mutations that seem to be responsible for frontotemporal dementia, more so than in Alzheimer's disease," Chow explained.
Most genetic FTD cases are caused by a mutation in one of three genes: C9ORF72, MAPT or GRN.
Chow noted that 30% to 40% of patients living with FTD carry these genetic mutations or variants.
"That's where genetic counseling becomes important," she said. "The genetic counselor will often talk about the pros and cons of knowing this information and run through the scenarios if the test comes out positive."
"When they said I had the option for genetic testing, I said, ‘Sign me up.’"
As soon as Nash’s father was diagnosed and Nash found out the condition was genetic, she knew she wanted to find out whether she was a carrier of the mutation.
"I needed to know, because for so many years, I wasn't in control," she told Fox News Digital. "I needed to make a plan. This was a chance to be in control of myself."
She added, "When they said I had the option for genetic testing, I said, ‘Sign me up.’"
Tough news leads to empowerment
When Nash found out in 2016 that she's a carrier of the gene mutation, she had mixed emotions.
On one hand, she was scared of what that might mean for her future.
"I did take it really hard when I first found out," she said. "It took years before I could speak about it publicly."
At first, Nash had processed the news as if it was a diagnosis. But over the years, she found that the knowledge helped her appreciate even the smallest details of day-to-day life.
"Now I feel empowered by this knowledge," Nash told Fox News Digital. "It's going to help more than I could possibly imagine. That flip of the brain was definitely needed."
Nash said she appreciates having the ability to share her discovery with her loved ones — the people who would be most affected, ultimately, if her predisposition led to a diagnosis down the road.
Nash said she is hopeful that dementia treatments may become available in time to benefit her.
"I wouldn’t want my worst enemy to have to go through what I went through without having the answers," she said.
Dementia treatments in the pipeline
Although there are therapies that can treat the symptoms of dementia — in an attempt to make people less anxious or less restless — there are no disease-modifying therapies currently approved by the FDA, Chow said.
"There are several experimental therapies being studied that are designed to target specific genetic mutations for FTD," said Chow.
Alector, the biotechnology company where Chow works in drug development, is currently running advanced clinical trials of a medication called latozinemab.
"Although it’s still under investigation, the drug may boost aspects of our system to clear the abnormal protein collections [in the brain] that are believed to cause FTD," Chow said.
Given her young age, Nash said she is hopeful that dementia treatments may become available in time to benefit her.
"That time difference presents an opportunity to apply a disease-modifying therapy once one has been approved, because the earlier you start a therapy that has been proven efficacious and safe, the better chance you have of not developing symptoms once you reach 50 or 60," Chow said.
"And that’s what makes it so empowering."
Ty is also optimistic about the potential for dementia treatments — not only by discovering new drugs, but also repurposing existing medications.
"In the next 10 years, I hope to see exciting changes in the way we detect, diagnose and treat dementia."
"A recent survey showed that there's a reluctance among physicians to have the conversation and do the testing because there’s this assumption that ‘there’s nothing we can do,’" she said. "But I think that's going to change with the introduction of some of these new therapeutics."
"In the next 10 years, I hope to see exciting changes in the way we detect, diagnose and treat dementia," she added.
There are also ways to delay dementia development through lifestyle modifications, Ty pointed out.
A 2020 study published in The Lancet identified 12 modifiable risk factors for dementia, including smoking, physical inactivity, social isolation, depression, air pollution, lack of education, hearing loss, traumatic brain injury, hypertension, high alcohol consumption, diabetes and obesity.
"If those were managed, you could reduce 40% of dementia worldwide," Ty said.
Looking ahead: ‘Excited for my future’
For those who are facing a similar struggle, Nash’s advice is to not bottle up all the emotions that come with it and to seek mental health care.
"Put your feelings out there," she recommended. "It's okay not to be okay at times. It’s a heavy thing to carry, but knowledge is power."
"You can make a plan," she went on.
"For me, I’m going to do everything I can to help people and to help myself."
For a long time after discovering her mutation, Nash had dwelled on the idea that she "only had so many years" before her dementia symptoms would begin. Over the past couple of years, however — with the help of her family support system and regular counseling sessions — she has adopted a new mindset.
"I found myself again," she said. "I have a gosh-darn future, and I can’t wait for it."
https://www.foxnews.com/health/iowa-woman-27-99-percent-chance-developing-dementia-needed-know