In 2019, doctors in London saw a 5-year old girl from rural
Ethiopia with an enormous tumor extending from her cheek to her lower jaw. Her
name was Negalem and the tumor was a vascular malformation, a life-threatening
web of tangled blood vessels.
Surgery to remove it was impossible, the doctors told the
foundation advocating for the girl. The child would never make it off the
operating table. After a closer examination, the London group still declined to
do the procedure, but told the child's parents and advocates that if anyone was
going to attempt this, they'd need to get the little girl to New York.
In New York City, on 64th street in Manhattan, is the
Vascular Birthmark Institute, founded by Milton Waner, MD, who has exclusively
treated hemangiomas and vascular malformations for the last 30 years. "I'm
the only person in the [United] States whose practice is exclusively [treating]
vascular anomalies," Waner tells Medscape.
Waner has assembled a multidisciplinary team of experts at
the institute's offices in Lenox Hill — including his wife Teresa O, MD, a
facial plastic and reconstructive surgeon and neurospecialist. "People
often ask how the hell do you spend so much time with your spouse?" Waner
says. "We work extremely well together. We complement each other."
O and Waner each manage half of the cases at VBI. And in
January they received an email about Negalem. After corresponding with the
child's advocate and reviewing images, they agreed to do the surgery, fully
aware that they were one of only a handful of surgical teams in the world who
could help her.
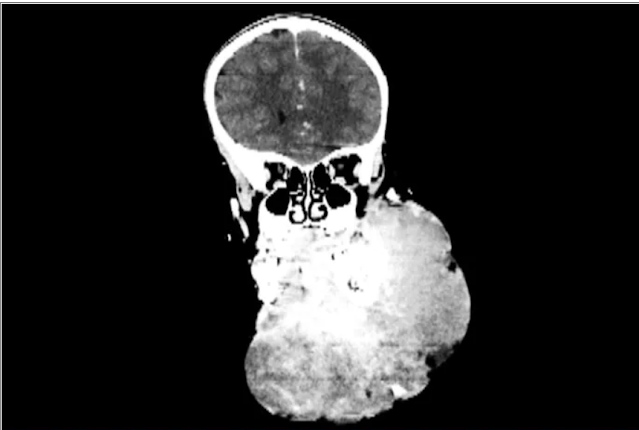
An image of a scan of the patient before
surgery.
The challenge with vascular malformations in children, Waner
says, is that they have a fraction of the blood an adult has. Where adults have
an average of 5 L of blood, a child this age has only 1 L. To lose 200 or 300
mL of blood, "that's 20 or 30% of their blood volume," Waner said. So
the removal of such a mass, which requires a meticulous dissection around many
blood vessels, carries a high risk of the child bleeding out.
There were some logistical hurdles, but the patient arrived
in Manhattan in mid-June, at no cost to her family. The medical visa was
organized by a volunteer who also work for USAID. Healing the Children
Northeast paid for her travel and the Waner Kids Foundation paid for her hotel
stay. Lenox Hill Hospital and Northwell Health covered all hospital costs and
post-surgery care. And Drs. O and Waner did the planning, consult visits, and
procedure pro bono.
The surgery was possible because of the generosity of
several organizations, but the two surgeons still had a limited time to remove
the mass. Under different circumstances, and with the luxury of more time, the
patient would have undergone several rounds of sclerotherapy. This procedure,
done by interventional radiologists, involves injecting a toxin into the blood
vessels which causes them to clot. Done prior to surgery it can help limit
bleeding risk.
On June 23, the morning of the surgery, the patient
underwent one round of sclerotherapy. However, it didn't have the intended
effect, Waner said, "because the lesion was just so massive."
The team had planned several of their moves ahead of time.
But this isn't the sort of surgery you'd find in a textbook. Because it's such
a unique field, Waner and O have developed many of their own techniques along
the way. This patient was much like the cases they treat every day, only
"several orders of magnitudes greater," Waner said. "On a scale
of 1 to 10 she was a 12."
Negalem, 5, before her surgery.
The morning of the surgery, "I was very
apprehensive," Waner recalled. He vividly remembers the girl's father repeatedly
kissing her to say goodbye as she lay on the operating table, fully aware that
this procedure was a life-threatening one. And from the beginning there were
challenges, like getting her under anesthesia when the anatomy of her mouth,
deformed by the tumor, didn't allow the anesthesiologists to use their typical
tubing. Then, once the skin was removed, it became clear how dilated and
tangled the involved blood vessels were. There were many vital structures
tangled in the anomaly. "The jugular vein was right there. The carotid
artery was right there," Waner said. It was extremely difficult to
delineate and preserve them, he said.
Once they got into the surgery they also realized that the
growth had adhered to the jaw bone. "There were vessels traversing into
the bone which were hard to control," O said.
But finally, both doctors realized they'd be able to remove
it. With the lesion removed they began the work of reconstruction and
reanimation.
The child's jaw and cheek bone had grown beyond their normal
size to support the growth. They had to shave them down to achieve facial
symmetry. The tumor had also inhibited much of the child's facial nerve
control. With it gone, O began the work of finding all the facial nerve
branches and assembling them to reanimate the child's face.
Before medicine, O trained as an architect, which, according
to Waner, has equipped her with very good spatial awareness — a valuable skill
in the surgical reconstruction phase. After seeing a lecture by Waner, she
immediately saw a fit for her unique interest and skill set. She did fellowship
training with Waner in vascular anomalies, and then went on to specialize in
facial nerve reanimation. The proof of O's expertise is Negalem's new,
beautiful smile, Waner said.
The surgery drew out over 8 hours, as long as a day of
surgeries for the two doctors. When O finally walked into the waiting room to
inform the family of the success, the first words out of the father's mouth
were, "Is my daughter alive?"
A growth like Negalem had is not compatible with a normal
life. Waner's mantra is that every child has the right to look normal. But this
case went beyond aesthetics. If the growth hadn't been removed, the child was
only expected to live 4 to 6 more years, Waner said. Without the surgery, she
could have suffocated, starved without the ability to swallow, or suffered a
fatal bleed..
O and Waner are uniquely equipped to do this kind of work,
but both are adamant that treating vascular anomalies is a multidisciplinary,
multimodal approach. Specialties in anesthesiology, radiology, lasers, facial
nerves — they are all critical to these procedures. And often patients with
these kinds of lesions require medical and radiologic interventions in addition
to surgery. In this particular case, from logistics to post-op, "it was a
lot of teamwork," O said, "a lot of international teams coming
together."
Though extremely difficult, "in the end the result was
exactly what we wanted," Waner said. Negalem can live a normal life. And
as for the surgical duo, both feel very fortunate to do this work. O said,
"I'm honored to have found this specialty and to be able to train with and
work with Milton. I'm so happy to do what I do every day."
"That's why we really took our time. We just went very
slowly and deliberately," O said. The blood vessels were so dilated that
their only option was to move painstakingly slow — otherwise a small nick could
be devastating.
But even with the slow pace the surgery was
"excruciatingly difficult," Waner said. And early on in the
dissection he wasn't quite sure they'd make it out. The sclerotherapy hadn't
done much to prevent bleeding. "At one point every millimeter or two that
we advanced we got into some bleeding," Waner said. "Brisk
bleeding."
The surgery drew out over 8 hours, as long as a day of
surgeries for the two doctors. When O finally walked into the waiting room to
inform the family of the success, the first words out of the father's mouth
were, "Is my daughter alive?"
A growth like Negalem had is not compatible with a normal
life. Waner's mantra is that every child has the right to look normal. But this
case went beyond aesthetics. If the growth hadn't been removed, the child was
only expected to live 4 to 6 more years, Waner said. Without the surgery, she
could have suffocated, starved without the ability to swallow, or suffered a
fatal bleed.
O and Waner are uniquely equipped to do this kind of work,
but both are adamant that treating vascular anomalies is a multidisciplinary,
multimodal approach. Specialties in anesthesiology, radiology, lasers, facial
nerves — they are all critical to these procedures. And often patients with
these kinds of lesions require medical and radiologic interventions in addition
to surgery. In this particular case, from logistics to post-op, "it was a
lot of teamwork," O said, "a lot of international teams coming
together."
Though extremely difficult, "in the end the result was
exactly what we wanted," Waner said. Negalem can live a normal life. And
as for the surgical duo, both feel very fortunate to do this work. O said,
"I'm honored to have found this specialty and to be able to train with and
work with Milton. I'm so happy to do what I do every day."
Donavyn Coffey is a freelance journalist who covers health
and the environment from her home in the Bluegrass. Her work has appeared in
Popular Science, Insider, and SELF.
https://www.medscape.com/viewarticle/954312