Kellie Carr and her 13-year-old son, Daniel, sat in the waiting room of a pediatric neurology clinic for yet another doctor’s appointment in 2012. For years, she struggled to find out what was causing his weakened right side. It wasn’t an obvious deficit, by any means, and anyone not paying close attention would see a normal, healthy teenage boy.
At that point, no one had any idea that Daniel had suffered a massive stroke as a newborn and lost large parts of his brain as a result.
“It was the largest stroke I’d ever seen in a child who hadn’t died or suffered extreme physical and mental disability,” said Nico Dosenbach, the pediatric neurologist at Washington University School of Medicine in St. Louis who finally diagnosed him using a magnetic resonance imaging (MRI) scan.
"If I saw the MRI first, I would have assumed this kid's probably in a wheelchair, has a feeding tube and might be on a ventilator," Dosenbach said. "Because normally, when a child is missing that much brain, it's bad."
But Daniel — as an active, athletic young man who did fine in school — defied all logic. Before the discovery of the stroke, his mother had noticed some odd mannerisms, such as zipping up his coat or eating a burger using only his left hand. When engaged, his right hand often served as club-like support instead of a dexterous appendage with fingers. Daniel excelled as a left-handed pitcher in competitive baseball, but his coach found it unusual that he would always switch the glove to his left hand when catching the ball.
Medical professionals tried to help — first his pediatrician, followed by an orthopedic doctor who sent him to physical therapy — but no one could figure out the root cause. They tried constraint-induced movement therapy, which forces patients to use the weaker arm by immobilizing the other in a cast, but Daniel soon rebelled and broke himself free.
“Everybody was telling me, ‘You got to use your right hand.’ I was a hardheaded child, and I was like, I’ll do it when I want to do it,” said Daniel, now 23, with a degree from a technical college. “I had a bunch of doctors saying a bunch of words that I didn’t understand. Then I saw Dr. Nico, who initially thought I was in the wrong place.”
In November 2012, Carr took her son to see Dosenbach as a last-ditch effort. She sent his office the three five-inch ring binders that made up Daniel’s extensive medical records well in advance. Dosenbach entered the room, took one look at Daniel and immediately backed out, excusing himself.
“He was like, ‘Sorry, I have the wrong room.’ We had never seen him before, so we didn’t know if that was our doctor. About three minutes later, he comes back and asks for Daniel,” Carr said. “Years later, Dr. Nico told me that he expected to see someone in a wheelchair.”
Even before proving it with an MRI scan, Dosenbach saw that Daniel’s condition had all the signs of perinatal stroke, or stroke that occurs in the first month after birth.
Perinatal stroke is not as rare as one might think, with a prevalence of 1 in 1,100 live births, and is associated with lifelong disabilities, including cerebral palsy, epilepsy, behavioral disturbances and learning deficits. The most common type is arterial ischemic stroke, where an artery in the brain becomes blocked, usually by a placental blood clot.
“The week around your birth is probably the most focused period of risk you’ll have for stroke in your whole life,” said Adam Kirton, director of the Calgary Pediatric Stroke Program. “If you take an 80-year-old diabetic smoker with hypertension, their risk within a week of their life with risk factors through the roof is actually three to four times lower than perinatal stroke.”
What gave it away in Daniel’s case was the preference for his left side — perinatal stroke, like adult stroke, often affects only one hemisphere of the brain — coupled with a mysterious illness he had as a newborn. Two weeks after birth, he was admitted to the hospital for diarrhea, vomiting and feeding issues. Doctors thought he had some kind of infection, but it was never confirmed.
“He was hooked up to all these machines as a baby, and his heart rate and blood pressure would suddenly drop,” his mother said. “By the end of his illness, I made a deal with God that I was willing to take whatever’s left of Daniel, as long as He let him live.”
Fortunately, he slowly began to recover, eating a little more at a time, and eventually returned home.
Soon afterward, Carr noticed that Daniel had a more active left hand and dragged his right leg while learning to walk, but she never imagined her son could have suffered a stroke.
”[He was] always strongly left-handed, even at 1 year old — that’s not normal, but most people don’t know that,” Dosenbach said. “You don’t really develop handedness until about 2.”
Daniel also heavily compensated for his right-side weakness as he got older. He became accustomed to doing things quickly and efficiently his own way, which sometimes meant ignoring his right side altogether. This lack of use worried Carr, and she started taking him to doctors who were largely puzzled by his condition, until that fateful meeting with Dosenbach.
He told Carr that, in his opinion, her son had experienced a small, left-sided perinatal stroke during that early illness. All the diarrhea and vomiting probably caused excessive fluid loss and a subsequent loss of blood volume. Not enough blood in the body meant more distant areas of the brain were denied oxygen delivery, and brain tissue starved of oxygen begins to die.
An MRI scan wasn’t necessary, Dosenbach told her, but Carr wanted hard proof. She didn’t believe it, finding herself in a sudden state of panic and shock. Her father had succumbed to a stroke some years earlier, and she couldn’t fathom what such a diagnosis meant for her young son.
“As a mother, I asked myself, ‘How the hell can you miss that? How could you not see it?’ ” she said. “And I was so hard on him about making sure he used his right hand more. It was just a horrible time. You just ride yourself so hard because you’ve missed such a catastrophic thing.”
What Dosenbach assumed would be a tiny, one-sided brain injury turned out to be much bigger.
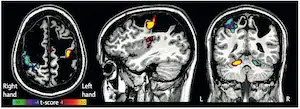
Structural MRI, which visualizes the size and shape of structures in the brain, revealed evidence of a massive stroke that targeted both hemispheres. Daniel was missing about a quarter of his cerebral cortex, the outer layer of the brain associated with higher level processes such as thought, memory, consciousness, language and movement.
The motor cortex, one of the principle areas involved in movement, is a U-shaped strip of brain tissue that goes down either side of the head. Daniel shockingly only has cerebrospinal fluid where much of the motor cortex should be. He also has no frontal eye fields on either side — the brain regions that control eye movement — even though he can move his eyes just fine. In April, Dosenbach and his colleagues published a case report on Daniel in the journal Lancet Neurology, detailing their findings.
Kirton, a pediatric neurologist who specializes in perinatal stroke but wasn’t involved in the research, has seen seemingly impossible cases such as Daniel’s before. Nevertheless, he agrees that Daniel’s accomplishments — being a star athlete in school, graduating from a technical college, and working in an automotive machine shop — are nothing short of amazing.
“Most kids who had big strokes on both sides don’t do well. They’re in a wheelchair and can’t walk, talk or use their hands — it can be extremely debilitating,” said Kirton, who recently co-founded the International Pediatric Stroke Organization (IPSO). “If I saw this MRI when he was a baby, I would have cautioned the parents that the most likely thing is that he’s going to have a lot of trouble. I certainly wouldn’t predict him to be a baseball player or working with his hands as an adult.”
So how was Daniel able to overcome such a major injury when so many of his peers did not? For the next four years, Daniel visited the lab weekly for more MRI scans — about 30 hours worth — to help Dosenbach and his colleagues uncover some answers. The researchers performed precision functional mapping on Daniel, which involves scanning the same person over and over to understand how the individual brain functions are organized.
In short, Daniel’s brain was able to remap itself to make up for all the lost tissue. All the functions are more or less still intact, but have shifted themselves around as compared with a healthy brain. For example, his lack of brain tissue where the left motor cortex should be meant that the activation area dedicated to movement had to be pushed further back, to a region typically reserved for processing sensory information. Daniel has only a thin sliver of tissue where the right motor cortex should be, yet it is somehow responsible for his incredibly dexterous left hand.
“There’s this interaction between the specific parts of his brain that were retained and when exactly the injury happened in his developmental trajectory that is ultimately going to explain how he ended up doing so well,” said Timothy Laumann, a psychiatrist at Washington University School of Medicine in St. Louis and member of Dosenbach’s lab. “His brain seems to be using its cortical sheet as best it can to represent the things that it needs.”
To support this plasticity hypothesis, Kirton said that a perinatal stroke often doesn’t affect language development, since babies that young haven’t yet installed the network for language in the brain. Even if they’ve suffered a large stroke in the regions where language would traditionally be mapped, children can recruit brain areas on the other side or even a completely different part of the brain. On the other hand, many more individuals have problems with movement after a perinatal stroke because the motor system is already partially installed at birth.
The research study gave Daniel, who now works as a sales porter at a car dealership, a new perspective on life and his condition.
He struggles with the same issues as most of his 23-year-old peers, such as becoming financially stable, buying a house and meeting a life partner. But Carr isn’t worried and, after finally receiving a diagnosis after 13 long years, she said she feels extremely proud of her son for surviving everything that he did.
“Daniel has ebbed and flowed like every other normal kid and just because he’s missing a huge chunk of his brain, that hasn’t stopped him,” his mother said. “He’s passed every hurdle put in front of him, either knocked it to the side or gone under it or over it, but he’s found a way to keep going.”
“Some days, I think to myself, ‘Wow, I’ll never be that normal person I tried to be for so long.’ That’s why I kept my condition a secret, so nobody would take a second look,” Daniel said. “It was hard, but it is what it is. I just take everything day by day, knowing that I’m not in the ground, and I’m not in a wheelchair.”
https://www.washingtonpost.com/health/perinatal-stroke/2022/01/21/7347c514-3903-11ec-91dc-551d44733e2d_story.html
Laumann TO, Ortega M, Hoyt CR, Seider NA, Snyder AZ, Dosenbach NU; Brain Network Plasticity Group. Brain network reorganisation in an adolescent after bilateral perinatal strokes. Lancet Neurol. 2021 Apr;20(4):255-256. doi: 10.1016/S1474-4422(21)00062-4. Epub 2021 Mar 17. Erratum in: Lancet Neurol. 2021 May;20(5):e4. PMID: 33743230.
[No abstract. Numerous figures in article.]
The large disparity between the extent of his brain injury and his functional status justified further investigation. PS1 scored within 2 SD of the mean of age-matched (15 years) standardised scores on intelligence quotient and cognitive function. Motor testing revealed a slight deficit of the right upper limb in strength, speed, and dexterity relative to the left upper limb.
No comments:
Post a Comment