Llenas-García J, Guerra-Vales JM, Alcalá-Galiano A, Domínguez C, Pérez-Nuñez A, Lizasoaín M, Díaz-Pedroche C, Montes S, Martínez J, Sierra F, Salto E. Cerebral neuroschistosomiasis: a rare clinical presentation and review of the literature. BMJ Case Rep. 2009;2009:bcr04.2009.1787. doi: 10.1136/bcr.04.2009.1787. Epub 2009 Aug 19. PMID: 21852999; PMCID: PMC3030161.
Abstract
The symptomatic presentation of cerebral schistosomiasis is
uncommon. The case of a 25-year-old woman from Equatorial Guinea with headache
and seizures secondary to cerebral neuroschistosomiasis, as confirmed by
histopathological examination and microbiological study, is presented. A review
of the literature on this subject is also provided.
From the article
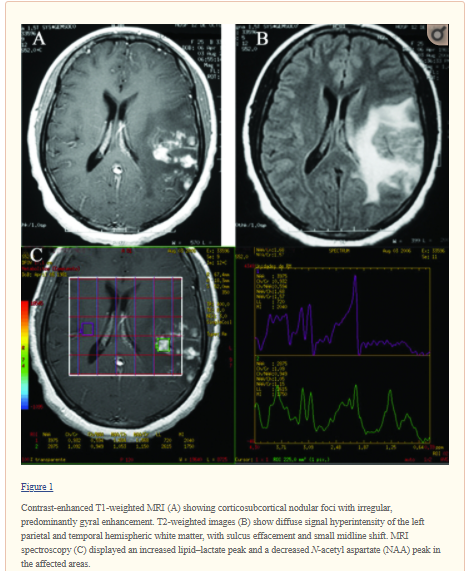
We present the
case of a 25-year-old woman from Equatorial Guinea. Her personal history was
relevant, with a typhoid fever episode in 2001 and two episodes of paludism,
the most recent in 2002. In March 2006 she presented with holocranial headache,
hyperesthaesia in her right hemibody and clonic seizures that started in the
right hemibody, secondarily generalised. There was no sign of fever or
constitutional syndrome. Brain CT showed space-occupying lesions in the left
cerebral hemisphere, and electroencephalogram (EEG) indicated epileptiform
activity of the Grand Mal type. Treatment with methylprednisolone and
phenobarbital was prescribed, and the patient became seizure free. The patient
was referred to our hospital for evaluation in July 2006…
The patient was
treated with phenytoin and dexamethasone from admission onward, with a
subsequent reduction of brain oedema, allowing for a lumbar puncture with the
following cerebrospinal fluid (CSF) test results: 5 leukocytes/mm3, 0 red blood cells (RBCs)/mm3, glucose 64 mg/dl, total proteins 0.28 g/litre and
intrathecal synthesis of IgG. CSF microbiology tests were all negative. Empiric
treatment was started with albendazole 400 mg every 12 h for 14 days, followed
by praziquantel 60 mg/kg/day in two daily doses for 2 days. The steroid dose
was progressively reduced after treatment, but 1 month later the patient again
presented with seizures; an MRI showed a new lesion in the left parasagital
parietal region. An open brain biopsy of this new lesion was carried out,
revealing a whitish and opaque thickened meninges coating an avascular nodular
white elastic tissue replacing the cerebral cortex. Histology revealed multiple
epithelioid granulomas formed around parasite ova. Some of the eggs had an
ovoid shape and were limited by a periodic acid-Schiff (PAS)-positive membrane,
a feature that permitted identification as Schistosoma ova. In conjunction with the ova, giant
multinucleated cells and a surrounding lymphocytic inflammatory infiltrate were
also observed. Several completely fibrosed granulomas were also identified (fig ).
Direct
microscopic examination was performed on fresh brain tissue, revealing Schistosoma spp. eggs. Treatment was initiated with oral
praziquantel 60 mg/kg/day in two daily doses for 3 days, and completed with
oral corticoid treatment in a slowly decreasing dose for an additional month.
The patient became asymptomatic. At 14 months later she is free of symptoms and
repeated MRI shows residual lesions.
Liu H, Lim CC, Feng X, Yao Z, Chen Y, Sun H, Chen X. MRI in cerebral schistosomiasis: characteristic nodular enhancement in 33 patients. AJR Am J Roentgenol. 2008 Aug;191(2):582-8. doi: 10.2214/AJR.07.3139. PMID: 18647936.
Abstract
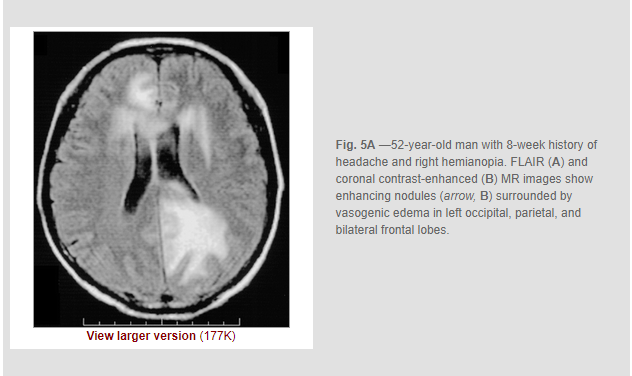
Objective: The purpose of our study was to describe the
characteristic MRI appearance of cerebral infection with Schistosoma japonicum.
Conclusion: Cerebral infection with S. japonicum can cause a
characteristic MRI pattern of a large mass comprising multiple intensely
enhancing nodules, sometimes with areas of linear enhancement. The typical
appearance may be useful for diagnosis in endemic regions and may potentially
be useful in cases imported into countries in which the disease is not endemic.
Courtesy of a colleague

No comments:
Post a Comment